OSAA Health & Safety
- Pre-Event Safety Timeout
- Air Quality
- Heat Index
- Emergency Action Plan
- Concussion
- Steroid and Supplements
- Heat / Hydration
- Sport Nutrition
- Student Wellness
- Lightning Safety
- Additional Resources
Pre-Event Safety Timeout
A Pre-Event Safety Timeout is designed to prepare site administrators, coaches, officials, athletic trainers, emergency medical services, team physicians, and anyone designated as responsible for the safety and medical well-being of athletes or spectators on game day to be aware, prepared, and educated.
What Is Included On The Pre-Contest Timeout Card (Front)?
Participants: The site supervisor, home/away coach(s), and official(s) should meet prior to the contest start to review the checklist questions in the event of an emergency or contest interruption. If present, the athletic director (AD), athletic trainer (AT), team physician, and EMS should be included in the meeting.
Checklist Questions: Review these questions with the participants of the Pre-Event Safety Timeout prior to each contest to ensure that all parties are on the same page.
- Who is the onsite contact for each school?
- Is there a qualified medical professional present? If not, who will lead in case of an emergency?
- Venue EAP: Who calls 911? Who meets EMS (and where)?
- Where's the nearest AED? Who will retrieve it?
- Environmental concerns? (heat index, air quality, lightning)
- Contest Interruption Policy: Cover policy and who officials are communicating with if behavior is reported to them
What Is Included On The Pre-Contest Timeout Card (Back)?
Emergency Information: The BACK of the pre-contest timeout card is for you to edit and include your venue/site specific information and important contacts. The form is fillable so you can provide your own information in the boxes. Include phone numbers of individuals that need to be contacted in the event of an emergency or situation. These individuals could include the athletic director, principal, security, school resource officer, athletic trainer, game manager, etc. Each school is unique as to who they have in attendance at a particular contest.
Venue Address: Include the general address for the contest (i.e. stadium, school, soccer field, etc.)
EMS Arrival: Include directions on how EMS will access your specific location.
FAQ
If there are multiple events occurring, should they each have a pre-event safety timeout?
Events at different venues should each have one (e.g., soccer and volleyball).
Events at the same venue may not need multiple meetings. For example, if JV and varsity play back-to-back, and the same personnel will be there, then another meeting is unneeded. However, if different individuals are responsible for responding to an emergency, then have another meeting.
How long should it take?
It depends on the school, the event, and the venue, but generally it should take less than a couple of minutes to answer the questions.
What happens if one or more of the questions cannot be answered?
The host school should work to correct any deficiencies. The OSAA Sports Advisory Committee can be consulted for help.
Emergency Action Plan (EAP)

Resources
» EAP Winter Practice Drills
» EAP Fall Practice Drills
» EAP Student Response Team Worksheet - Fillable Form
» EAP Campaign Online Feedback Form
» EAP - Basic Template
» Emergency Equipment Example
» Communication Plan Example
» First Responder Roles Example
» EAP Best Practices Checklist
» Venue Directions Example
» OSAA Board Policy - Emergency Action Plan
» NFHS Recommendations and Guidelines for Minimizing Head Impact Exposure and Concussion Risk in Football
» National Athletic Trainers’ Association: Emergency Planning in Athletics
» Anyone Can Save a Life Program
EAP Campaigns
2023-24 Campaign
» Article 2 - Team Worksheet & Event Staff - Sep. 7
» Article 3 - Fall Drills - Oct. 12
» Article 4 - Winter Introduction - Nov. 17
» Article 5 - Spring Introduction - March 4
» Article 6 - Recognizing Cardiac Collapse - March 22
» Article 7 - Working With Local EMS - April 12
» Article 8 - Large Event EAP - June 13
2019 Campaign
» Article 2 - Venue Directions & Emergency Transport - Jan. 3
» Article 3 - Emergency Personnel - Jan. 29
» Article 4 - Emergency Communication - March 15
» Article 5 - Emergency Equipment - May 2
» Article 6 - Additional Considerations for Emergency Planning - June 7
Oregon Athletic
Trainers Society
NFHS
Sports Medicine
OSAA Health and Safety Information
The information listed on this page is designed to assist schools, parents, and students in keeping student-athletes healthy and safe when dealing with a variety of issues. We encourage you to contact the OSAA staff directly (info@osaa.org) if you have questions regarding the following information.
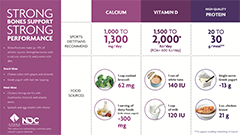
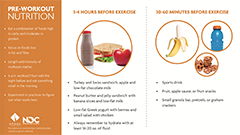
Sport Nutrition
» Eating for Peak Performance
» Sports Nutrition Information Center - USDA
» Top 5 Nutrition Needs for Student Athletes
Sports Nutrition Instagraphics
From recovery nutrition to bone health to lactose intolerance and hydration, these instagraphics provide sports dietitian-recommended tips and short descriptions of the important points on eight topics.NFHS Concussion in
Sports Training Course
Concussions and Concussion Management
» Oregon Department of Education (ODE) Brain Injury Procedures
» Immediate Temporary Accommodations Plan (ITAP)
» ODE Return to School after a Concussion or Other Brain Injury Resources
» Qualified Health Care Professional (ORS 336.490)
» Medical Release - Return to Participation Medical Release Following a Concussion
» OSAA Athletic Director and Coach Requirements
» OATS Concussion for Schools without an Athletic Trainer
» Concussion - Private School Informed Consent Form
» The Center on Brain Injury Research and Training (CBIRT)
» CBIRT Return to Academics Protocol After Concussion
» CBIRT Academic Accommodations Matrix
» CBIRT Post-Concussion Academic Accommodation Protocol
» Oregon Concussion Awareness and Management Program (OCAMP)
» Returning to Learn Following a Concussion
» CDC Heads Up Website
» A Parent's Guide to Concussions
» NFHS Suggested Guidelines for Management of Concussion in Sports
» OSAA Concussion Information and Sideline Concussion Guide
Questions and Answers about Return to Play
A.Oregon law requires the:
1. The athlete no longer exhibits signs, symptoms, or behaviors consistent with a concussion
and
2.Recieves a medical release from a "qualified" Health Care Professional.
Q. Who is considered a "qualified" Health Care Professional?
A. A physician (M.D. or D.O.), Physician Assistant (PA), Nurse Practitioner (NP), or Psychologist licensed or certified in Oregon can provide a medical release. Other professionals include: Chiropractic Doctor (DC), Naturopathic Doctor (ND), Physical Therapist (PT), and Occupational Therapist (OT).
Q. Can an athlete with a suspected concussion return to participate on the day of the injury?
A. Any athlete suspected of a concussion must be removed from play immediately and cannot return to play until receiving a release from a medical profession no sooner that the following day, with one exception. If an athletic trainer or physician licensed or registered in Oregon determines that the athlete has not suffered a concussion the athlete may return to play that day.
Q. How quickly can the athlete return to play following a concussion?
A. Best practice recommends the athlete complete a gradual return to participation protocol. This is a 6-step process with each step increasing exertional demands on the athlete.
OSAA Steroids Training
and Assessment Information
Steroids and Supplements
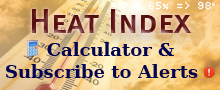
Heat Illness and Hydration
» OSAA Heat Index Calculator, Policies, & Practice Model
» OSAA Heat Index Policy
» NFHS Guide to Heat Acclimatization and Heat Illness Prevention Course
» NFHS Fluid Replacement and Dehydration Information
» NFHS Heat-Related Illness Information
» NFHS Position Statement and Recommendations for Hydration to Minimize the risk for Dehydration and Heat Illness
» NFHS Position Statement on Energy Drinks
» NFHS Position Statement on Heat Acclimatization and Heat Illness Prevention
» Heat Stress Information
» Hydration Guidelines
» First-Aid for Heat Illness
» Extreme Heat and Public Health
» Heat and Your Health
» CDC Course on heat related illness
» Heat Related Illness geared to Athletics
Cold-Related Illness
Air Quality Guidelines
These guidelines, created in consultation with the Oregon Health Authority (OHA) and the Oregon Department of Environmental Quality (DEQ), provide a default policy to those responsible or sharing duties for making decisions concerning the cancelation, suspension, and/or restarting of practices and contests based on poor air quality.
A. Designate Personnel: Given the random behavior of wind and air currents, air quality may change quickly. Schools shall designate someone who will monitor the air quality prior to and during outdoor activities. While typically due to wildfires, schools need to also consider non-wildfire situations if the air quality is unhealthy.
B. Areas With Air Reporting Stations: The Air Quality Index (AQI) should be monitored throughout the day, and during an event, to have the best data possible to make informed decisions about conducting practices and competitions. Schools should always defer to the monitor that is the nearest physical distance to the practice or contest facility. School personnel shall review the AQI information for all regions throughout the state to determine if action is necessary (see chart below). Schools shall regularly review the AQI throughout events to assess deteriorating conditions. School personnel shall use the AirNow Fire and Smoke map at https://fire.airnow.gov/. This map shows larger circles with numbers for DEQ/AirNow monitors and smaller circles with no letters or numbers for PurpleAir sensors. The EPA applies a series of quality control checks and an extended U.S.-wide correction equation before displaying the PurpleAir sensor data on the Fire and Smoke map to provide data more consistent with permanent monitors.
C. Areas Without Air Reporting Stations: If air monitoring equipment is not available, member schools should utilize the 5-3-1 Visibility Index to determine air quality.
-
5-3-1 Visibility Index: Making visual observations using the 5-3-1 Visibility Index is a simple way to estimate air quality and know what precautions to take. While this method can be useful, you should always use caution and avoid going outside if visibility is limited, especially if you are sensitive to smoke.
- Determine the limit of your visual range by looking for distant targets or familiar landmarks such as mountains, mesas, hills, or buildings at known distances. The visual range is that point at which these targets are no longer visible. As a rule of thumb: If you can clearly see the outlines of individual trees on the horizon it is generally less than five miles away. It is highly recommended that schools use pre-determined landmarks that were established on a clear day to determine their visual range.
- Ideally, the viewing of any distant targets should be made with the sun behind you. Looking into the sun or at an angle increases the ability of sunlight to reflect off of the smoke, thus making the visibility estimate less reliable.
- Be aware that conditions may change rapidly and always use the more conservative of multiple metrics (AQI, 5-3-1 Visibility Index, etc.).
Visibility Distances

D. Act: This chart will help determine the action needed based on the air quality in your area.
| Air Quality Index (AQI) | 5-3-1 Visibility Index | Required Actions for Outdoor Activities |
| 51 - 100 | 5-15 Miles | Athletes who are unusually sensitive to air pollution should consider indoor activities only. Athletes with asthma should have rescue inhalers readily available and pretreat before exercise if directed by their healthcare provider. All athletes with respiratory illness, asthma, lung or heart disease should monitor symptoms and reduce/cease activity if symptoms arise. Increase rest periods as needed. |
| 101 - 150 | 3-5 Miles | Athletes who are unusually sensitive to air pollution should consider indoor activities only. Athletes with asthma should have rescue inhalers readily available and pretreat before exercise if directed by their healthcare provider. All athletes with respiratory illness, asthma, lung or heart disease should monitor symptoms and reduce/cease activity if symptoms arise. Athletes with asthma or other lung diseases, heart conditions or diabetes may need additional rest breaks during practices / contests. Consider rescheduling to a different time and / or an area with a lower AQI. Schools should consider the impact of elevated AQI lasting for multiple days and the impact of prolonged exposure for athletes and staff on multiple practice session days when making decisions. Consider moving practices indoors, if available. Be aware that, depending on a venue’s ventilation system, indoor air quality levels can approach outdoor levels. |
| 151 - 200 | 1-3 Miles | All outdoor activities (practice and competition) shall be canceled or moved to an area with a lower AQI. Move practices indoors, if available. Be aware that, depending on a venue’s ventilation system, indoor air quality levels can approach outdoor levels. |
| >200 | 1 Mile | All outdoor activities (practice and competition) shall be canceled or moved to an area with a lower AQI. Move practices indoors, if available. Be aware that, depending on a venue’s ventilation system, indoor air quality levels can approach outdoor levels. |
E. Additional Resources: Schools may also refer to OHA's fact sheet regarding School Outdoor Activities During Wildfire Events at https://apps.state.or.us/Forms/Served/le8815h.pdf.
F. Oregon Occupational Safety and Health Administration (OSHA) Rules: Schools should familiarize themselves with Oregon OSHA permanent rules adopted in Summer 2022 regarding reducing heat and wildfire smoke outdoor workplace exposure for employees. OSHA resources can be accessed here for Heat – https://osha.oregon.gov/Pages/topics/heat-stress.aspx and Wildfires https://osha.oregon.gov/Pages/topics/wildfires.aspx.
Student Wellness
Oregon Youth Suicide Awareness Campaign
National Suicide Prevention Lifeline
1-800-273-8255 (TALK)Crisis Text Line
Text TALK to 741741Call to Action for School
» Suicide PreventionEquip your coaches, athletic directors, and adult advisors for
extra-curricular activities in suicide prevention as student
athletes return to play.
Articles
» Article 1 - Awareness Campaign
» Article 2 - Bullying
» Article 3 - Identifying Suicide Warning Signs
» Article 4 - Talking About Suicide
» Article 5 - Suicide Prevention Resources
» Article 6 - Suicide Prevention Month
» Article 7 - Your Role in Responding to Suicide
Resources
» Challenges of Mental-health Issues in High School Athletics
» Student Mental Health and Suicide Prevention Course
» After a Suicide: A Toolkit for Schools
» American Foundation for Suicide Prevention
» Lines for Life
» Suicide Prevention Resource Center
» Suicide Prevention Poster
Lightning Safety Guidelines
A. These guidelines provide a default policy to those responsible or sharing duties for making decisions concerning the suspension and restarting of practices and contests based on the presence of lightning or thunder.
B. Proactive Planning:
- Assign staff to monitor local weather conditions before and during practices and contests.
-
Develop an evacuation plan, including identification of appropriate nearby safe areas and determine the amount of time needed to get everyone to a designated area.
- A designated safer place is a substantial building with plumbing and wiring where people live or work, such as a school, gymnasium, or library. An alternate safer place for the threat of lightning is a fully enclosed (not convertible or soft top) metal car or school bus.
-
Develop criteria for suspension and resumption of play:
- When thunder is heard or a cloud-to-ground lightning bolt is seen*, the leading edge of the thunderstorm is close enough to strike your location with lightning. Suspend play for at least 30 minutes and vacate the outdoor activity to the previously designated safer location immediately.
- Thirty-minute Rule: Once play has been suspended, wait at least 30 minutes after the last thunder is heard or flash of lightning is witnessed * prior to resuming play.
- Any subsequent thunder or lightning* after the beginning of the 30-minute count will reset the clock and another 30-minute count should begin.
- When lightning detection devices or mobile phone apps are available, this technology could be used to assist in making a decision to suspend play if a lightning strike is noted to be within 10 miles of the event location. However, you should never depend on the reliability of these devices and, thus, hearing thunder or seeing lightning* should always take precedence over information from a mobile app or lightning detection device.
- Review annually with all administrators, coaches, and game personnel and train all personnel.
- Inform student athletes of the lightning policy at start of season.
C. For more detailed information, refer to the "Lightning and Thunder Safety" section contained in the NFHS Sports Medicine Handbook.
Additional Sports Medicine Resources
OSAA Sports Medicine Advisory Committee Resources
Oregon Health Authority / OSAA Sports Medicine Advisory Committee Information
» Murmur Evaluation, Marfan's Screen, Musculoskeletal Exam Protocols
(Protocol videos to be posted soon.)
Pre-Participation Physical Exam Forms
Languages: English | Spanish | Chinese | Vietnamese | Russian
Infection Control
» MRSA in Sports Participation - Position Statement and Guidelines
» Sports Related Skin Infections - NFHS Position Statement
» MRSA Identification and Prevention - School Checklist
» EPA's Registered Products Effective Against Methicillin Resistant Staphylococcus aureus (MRSA)
» Sports Hygiene - Guidelines to Minimize Infectious Diseases
» Herpes Gladiatorum - Position Statement and Guidelines
» Communicable Skin Conditions - Practical Recommendations for Wrestling
» National Wrestling Coaches Association Skin Infection Resources
NFHS Sports Medicine Advisory Committee (SMAC) Resources
» NFHS Cold-Related Illness Information
» NFHS Position Statement - Air Quality April 2023
» NFHS Position Statement - Physical Activity, Air Quality and Wildfires
» NFHS Position Statement - Maintaining Hydration to Optimize Performance and Minimize the Risk for Exertional Heat Illness April 2022
» NFHS Position Statement - Heat Illness Prevention April 2022
» NFHS Position Statement - Emerging Technology May 2020
» NFHS Position Statement - Smokeless Tobacco May 2020
» NFHS Position Statement - Invasive Medical Procedures May 2020
» NFHS Position Statement - Appearance and Performance Enhancing Druge May 2020
» NFHS Position Statement - Sport Specialization August 2019
» NFHS Position Statement - Medical Devices August 2019
» NFHS Position Statement - Soft Headgear August 2019
» NFHS Position Statement - Soccer Headgear
» NFHS Position Statement - Invasive Medical Procedures
» NFHS Position Statement - Use of Mouthguards
» NFHS Position Statement - Emergency Action Plan (EAP) for Interscholastic Activities
» NFHS “Heat Illness Prevention” Online Course from NFHSLearn.com
» NFHS “The Collapsed Student” Online Course from NFHSLearn.com
» NFHS “Sudden Cardiac Arrest” Online Course from NFHSLearn.com
» NFHS “Emergency Action Planning for Afterschool Programs” Online Course from NFHSLearn.com
Sports Medicine and Medical Related Organizations
Follow the links below for additional sports medicine and medical related information.» American Academy of Pediatrics (AAP)
» American Academy of Family Physicians
» American College of Sports Medicine (ACSM)
» American Medical Society for Sports Medicine (AMSSM)
» American Orthopaedic Society of Sports Medicine (AOSSM)
» Centers for Disease Control and Prevention (CDC)
» Joint Commission on Sports Medicine and Science
» National Athletic Trainers Association (NATA)
» National Operating Committee on Standards for Athletic Equipment (NOCSAE)
» NCAA Health and Safety Information
» Sporting Good Manufacturers Association (SGMA)
Links
» NFHS Sickle Cell Trait Information
» Female Athlete Triad Information
» Addiction Treatment Information
» Alcohol & Drug Treatment Information
» Drug Abuse and Bullying
» Vaping Information
» DrugRehab.com
» RehabNet.com
» HealthCorps: Nonprofit for Teen Health
» U.S. Dept. of Health and Human Services - Talking with Teens
» Addiction Guide